Mouse study suggests a common diabetes drug may prevent leukaemia
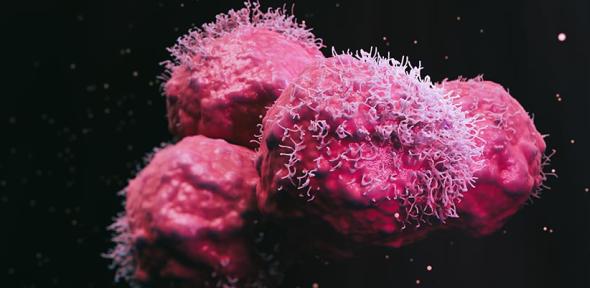
Around 3,100 people are diagnosed with acute myeloid leukaemia (AML) each year in the UK. It is an aggressive form of blood cancer that is very difficult to treat. Thanks to recent advances, individuals at high risk of AML can be identified years in advance using blood tests and blood DNA analysis, but there’s no suitable treatment that can prevent them from developing the disease.
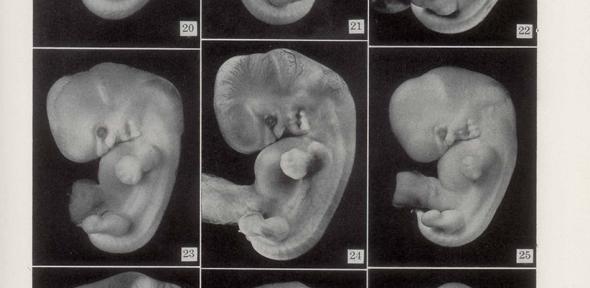
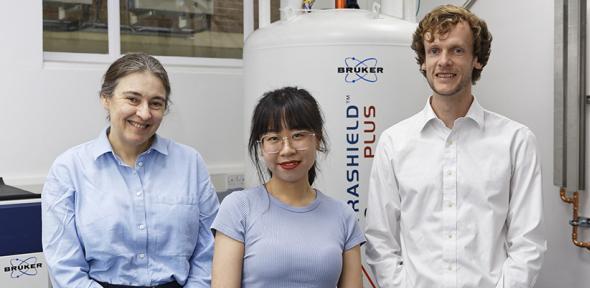
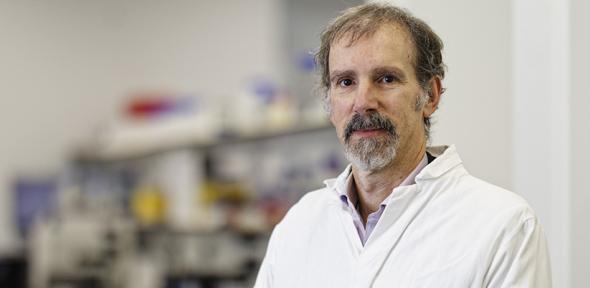
In this study, Professor George Vassiliou and colleagues at the University of Cambridge investigated how to prevent abnormal blood stem cells with genetic changes from progressing to become AML. The work focused on the most common genetic change, which affects a gene called DNMT3A and is responsible for starting 10-15% of AML cases.
Professor Vassiliou, from the Cambridge Stem Cell Institute at the University of Cambridge and Honorary Consultant Haematologist at Cambridge University Hospitals NHS Foundation Trust (CUH) co-led the study. He said: “Blood cancer poses unique challenges compared to solid cancers like breast or prostate, which can be surgically removed if identified early. With blood cancers, we need to identify people at risk and then use medical treatments to stop cancer progression throughout the body.”
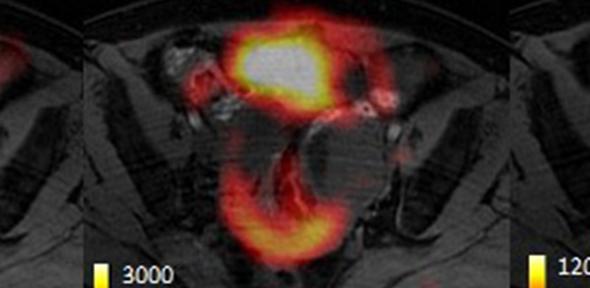
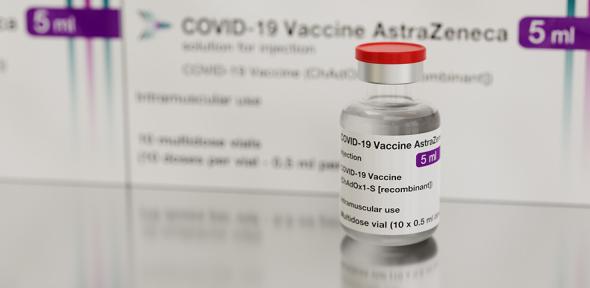
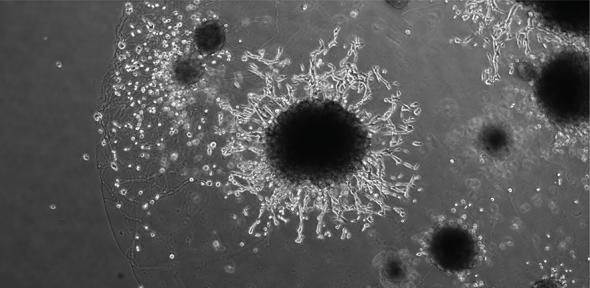
The research team examined blood stem cells from mice with the same changes in DNMT3A as seen in the pre-cancerous cells in humans. Using a genome-wide screening technique, they showed that these cells depend more on mitochondrial metabolism than healthy cells, making this a potential weak spot. The researchers went on to confirm that metformin, and other mitochondria-targeting drugs, substantially slowed the growth of mutation-bearing blood cells in mice. Further experiments also showed that metformin could have the same effect on human blood cells with the DNMT3A mutation.
Dr Malgorzata Gozdecka, Senior Research Associate at the Cambridge Stem Cell Institute and first author of the research said: “Metformin is a drug that impacts mitochondrial metabolism, and these pre-cancerous cells need this energy to keep growing. By blocking this process, we stop the cells from expanding and progressing towards AML, whilst also reversing other effects of the mutated DNMT3A gene.”
In addition, the study looked at data from over 412,000 UK Biobank volunteers and found that people taking metformin were less likely to have changes in the DNMT3A gene. This link remained even after accounting for factors that could have confounded the results such as diabetes status and BMI.
Professor Brian Huntly, Head of the Department of Haematology at the University of Cambridge, Honorary Consultant Haematologist at CUH, and joint lead author of the research, added: “Metformin appears highly specific to this mutation rather than being a generic treatment. That specificity makes it especially compelling as a targeted prevention strategy.
“We’ve done the extensive research all the way from cell-based studies to human data, so we’re now at the point where we have a made a strong case for moving ahead with clinical trials. Importantly, metformin’s lack of toxicity will be a major advantage as it is already used by millions of people worldwide with a well-established safety profile.”
The results of the study, funded by Blood Cancer UK with additional support from Cancer Research UK, the Leukemia & Lymphoma Society (USA) and the Wellcome Trust, are published in Nature.
Dr Rubina Ahmed, Director of Research at Blood Cancer UK, said: “Blood cancer is the third biggest cancer killer in the UK, with over 280,000 people currently living with the disease. Our Blood Cancer Action plan shed light on the shockingly low survival for acute myeloid leukaemia, with only around 2 in 10 surviving for 5 years, and we urgently need better strategies to save lives. Repurposing safe, widely available drugs like metformin means we could potentially get new treatments to people faster, without the need for lengthy drug development pipelines.”
The next phase of this research will focus on clinical trials to test metformin’s effectiveness in people with changes in DNMT3A at increased risk of developing AML. With metformin already approved and widely used for diabetes, this repurposing strategy could dramatically reduce the time it takes to bring a new preventive therapy to patients.
Tanya Hollands, Research Information Manager at Cancer Research UK, who contributed funding for the lab-based screening in mice, said: “It's important that we work to find new ways to slow down or prevent AML in people at high risk. Therefore, it’s positive that the findings of this study suggest a possible link between a commonly-used diabetes drug and prevention of AML progression in some people. While this early-stage research is promising, clinical trials are now needed to find out if this drug could benefit people. We look forward to seeing how this work progresses.”
Reference
Gozdecka, M et al. Mitochondrial metabolism sustains DNMT3A-R882-mutant clonal haematopoiesis. Nature; 16 Apr 2025; DOI: 10.1038/s41586-025-08980-6
Adapted from a press release from Blood Cancer UK
Metformin, a widely used and affordable diabetes drug, could prevent a form of acute myeloid leukaemia in people at high risk of the disease, a study in mice has suggested. Further research in clinical trials will be needed to confirm this works for patients.
![]()
The text in this work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. Images, including our videos, are Copyright ©University of Cambridge and licensors/contributors as identified. All rights reserved. We make our image and video content available in a number of ways – on our main website under its Terms and conditions, and on a range of channels including social media that permit your use and sharing of our content under their respective Terms.